What treatment options may
be available?
Following a relapse diagnosis, healthcare teams will explain what the treatment options may be.
Although active treatment options may be more limited after a relapse, there are several options available, depending on the type of AML and other eligibility factors such as age and fitness. Different treatments can require more or less time in hospital, and this will also be something to consider. We have summarised the most common available treatments below.
Prioritising your needs:
While healthcare teams will help guide treatment decisions, it is important to remember that any final choices sit with those who have relapsed and their loved ones.
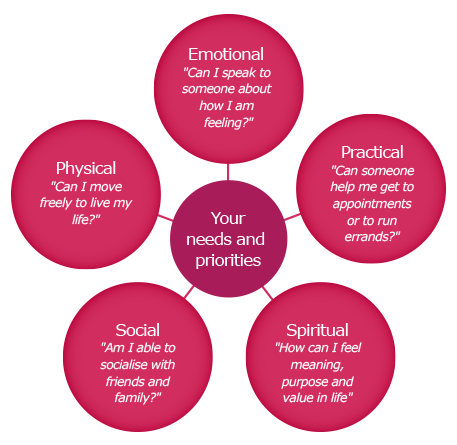
It is a good idea to think first about your personal life objectives and needs and what you would like to get from your treatment. This is so you can discuss with your healthcare team how they can work with you to ensure your priorities are fully met:
Bone marrow transplant
A bone marrow, or stem-cell transplant, may be an option based on eligibility factors such as age, general health, availability of a donor, response to previous treatments and the support system available for you both pre- and post-transplant.5,6 Read more about bone marrow transplants here.
Chemotherapy and targeted therapies
Additional rounds of chemotherapy, as well as targeted therapies such as an oral treatment, can also be offered as an option for treatment.1 Your eligibility for these treatments will again be reviewed by your healthcare team.
Other treatment options
Clinical trials are used to research potential new treatments and tests. The criteria for taking part in a clinical trial are very specific, but healthcare teams will be able to advise whether you would be eligible for any relapse-specific trials within your region.
Holistic support: some people seek alternative or holistic treatment options outside of a hospital setting. Always discuss these with your healthcare team who can factor this into your ongoing care.
Ongoing symptom management (palliative care)
In some cases, your doctor may recommend that treatment options aimed to achieve remission may no longer be viable as the best option or may not be the best choice for your personal priorities in the long run. This does not mean that nothing can be done. In this situation, healthcare teams will focus on prioritising your physical, practical, social and emotional needs, through what is called ‘palliative care’.7
While the term palliative care may be scary to hear, it is important to know that the definition has evolved significantly over the years, and it is not the same as terminal care.7 The NHS now defines palliative care as an approach that aims to improve quality of life for people living with AML and their families, and is increasingly being referred to as ongoing symptom management.7

This approach focuses on prioritising your quality of life, preventing and relieving suffering through the early identification, correct assessment and treatment of pain, and other problems.Your healthcare team may recommend pain-relief (analgesics), nausea-relief (anti-emetics), antidiarrhoeals and transfusions, in order to alleviate symptoms.7 Chart medication from your home so hospital admissions are avoided.
It is important to know that palliative care can improve how you cope with AML day to day, with reduced symptoms through pain relief for example, you can enjoy daily activities such as walking in the park and visiting family, which may not have been possible without this care.
When considering palliative care, it is a good time for you and your loved ones to reflect and think about your personal needs and priorities, and what you would like to achieve from treatment. Map out your priorities, as in the diagram above, and discuss this with your healthcare team. They will work with you to find a plan for symptom management that best suits you.
Having all the information you need
Your healthcare team will provide their options and recommendations, however the final decision about your treatment will always be yours. Therefore, it is important to ask the right questions and feel like you have all the information needed to make these decisions.
The following checklist of questions may be useful to take with you to your next consultation, to help guide you in conversations with your healthcare team:
If there are any words or terms you don’t understand, our Terminology Explained document can help guide you.
References
1. Leukaemia Care. Relapse in Acute Myeloid Leukaemia (AML). https://media.leukaemiacare.org.uk/wp-content/uploads/Relapse-in-Acute-Myeloid-Leukaemia-AML-Web-Version.pdf [Last accessed November 2022].
2. Medical News Today. AML relapse: What it means and treatment options. https://www.medicalnewstoday.com/articles/aml-relapse [Last accessed November 2022].
3. Hourigan CS, Karp JE. Minimal residual disease in acute myeloid leukaemia. Nat Rev Clin Oncol. 2013;10(8):460–471.
4. Thol F, Gancer A. Treatment of Relapsed Acute Myeloid Leukaemia. Curr Treat Options Oncol. 2020;21(8):66.
5. Saultz JN, Garzon R. Acute Myeloid Leukemia: A Concise Review. J Clin Med. 2016;5(3):33.
6. Gregory TK, Wald D, Chen Y, et al. Molecular prognostic markers for adult acute myeloid leukaemia with normal cytogenetics. J Hematol Oncol. 2009;2:23.
7. NHS inform. Palliative care. https://www.nhsinform.scot/care-support-and-rights/palliative-care [Last accessed November 2022].
MAT-UKE-NON-2022-00013 | February 2023

